Abstract
Introduction: MDS is the second most common indication for Allo HSCT exceeded only by AML. For patients with transfusion dependence, hypoplastic, fibrotic or high-risk MDS allogeneic stem cell transplantation is offered as a potential cure. Many patients are elderly and may have older siblings, co-morbidities and tolerate GVHD poorly. The availability of mismatched related (MMR) donors has been described in patients with MDS with small singe centre series suggesting that the lower levels of acute and chronic GVHD may make these a desirable donor. We therefore studied the MDS patients in the EBMT database (DB) to understand the effect of donor on outcomes.
Methods: The EBMT DB has 3924 MDS patients transplanted between 1998- 2016. Patients transplanted between Jan 2011 and September 2015 from a matched related donor (MRD), 10/10 matched unrelated donor (MUD) or MMR donor with post transplant Cyclophosphamide (PT-CY) as GVHD prophylaxis and had data as part of the data quality initiative were included. Where continuous progression occurred the time to relapse was imputed as 4 weeks. Analysis was performed using SPSS v 23.0, OS and RFS were calculated by the Kaplan Meier method and multivariate analysis with Cox regresssion analysis
Results: Six hundred and nine patients with MDS, 163 (27%) MRD, 235 (38%) MMR and 211 (35%) MUD donors were included. The median age of recipients was 60 years (18-78 yr), transplanted at a median of 10 (0.6-314) months from diagnosis. The donors were male in 57% MRD, 58% MMR and 61% of MUD donors. High risk disease based on excess blasts occurred in 92/163 MRD (56%), 126/235 MMR (54%) and 133/211 (63%) MUD (p=0.01). At allograft 42 (27%) MRD, 67 (30%) MMR and 38 (18%) of MUD were in complete remission (p=0.014). Recipient/Donor combinations were Male/Male in 35% MRD, 40% MMF and 52% MUD; Male/Female in 22% MRD, 18% MMF and 10% MUD; Female/Male in 18% MRD, 28% MMR and 28% MUD; Female/Female in 25% MRD,15% MMR and 10% MUD (p=0.0); CMV status was R/D -/- in 22% MRD, 16% MMF and 36% MUD; -/+ in 18% MRD, 4% MMR and 10% MUD; +/- in 16% MRD, 22% MMR and 19% MUD; +/+ in 44% MRD, 38% MMR and 35% MUD (p=0.0). Conditioning regimes included ATG in 46% MRD, 4% MMR and 67% MUD (p=0.0); Campath in 4% MRD, <1% MMR and 8% MUD donors (p=0.0) and PT-CY was used in 1% MRD, 100% MMR and 1% MUD donors (p=0.0). Conditioning was myeloablative (MA) in 35% MRD; 49% MMR and 26% MUD; reduced intensity (RIC) in 65% MRD, 52% MMR and 74% MUD (p=0.0). TBI was administered in 13% MRD, 25% MMR and 5% MUD (p=0.0).
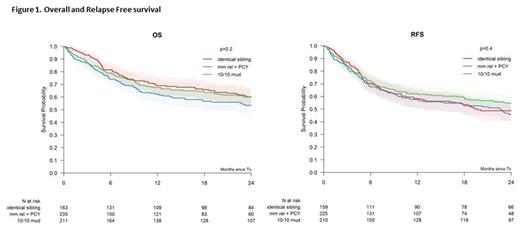
Neutrophil engraftment occurred in 96% MRD, 87% MMR and 92% MUD (p=0.004). Primary/secondary graft failure occurred in 1%/3% MRD, 10%/4% MMR and 4%/3% MUD. The cumulative incidence of engraftment of neutrophils at 100 days was 96% (95% CI: 93-99%) for MRD, 91% (95% CI 87-95%) for MMF and 93% (95% CI 90-97%) for MUD (p<0.001). A complete remission was achieved in 91% MRD, 89% MMR and 92% MUD (p=0.51). The cumulative incidence of aGHVD grade 2-4 at 100 days was 28% (95% CI: 21-35%) in MRD, 21% (95% CI: 16-27%) in MMR and 34% (95% CI: 27-40%) in MUD transplants (p=0.02). The incidence of extensive cGVHD at 2 years was 28% (95% CI: 21-35%) in MRD; 14% (95% CI 8-19%) in MMR and 31% (95% CI 24-37%) in MUD (p<0.001). The incidence of relapse with MRD was 30% (95% CI: 22-37%); MMR 26% (95% CI: 20-33%) and MUD 22% (95% CI: 16-27%) (p=.124). Overall survival (OS) at 2 years was 60% (95% CI:53-68%) for MRD, 53% (95% CI: 46-61%) for MMR and 60% (95% CI: 53-67%) for MUD (p=0.2). Relapse free survival (RFS) at 2 years was 49% (95% CI: 41-57%) for MRD, 46% (95% CI: 38-53%) for MMR and 55% (95% CI 48-62%) for MUD (p=0.4). On multivariate analysis age HR 1.01 (p=0.01) and MMF donor HR 1.55 (P=0.04) affected OS, MUD donors HR 0.6 (p=0.03) lowered relapse and MMR HR 0.6 (p=0.04) had lower cGVHD. There was no effect of time to transplant, RIC vs MA conditioning, T cell depletion or IPSS high on OS, RFS, relapse or NRM.
Conclusion: This large recent dataset of MDS patients includes MMF donors exclusively transplanted with PT-CY and demonstrates that OS for patients transplanted with MRD, MMR and MUD are similar whereas relapse may be lower with MUD transplants. As with other studies chronic extensive GVHD is lower with the MMR PT-CY approach, but the heterogeneity with respect to disease risk and status at transplant, limit conclusions regarding relapse free survival. These data need prospective validation to revalidate our current donor algorithms.
Raj: Mallinckrodt: Speakers Bureau; Bloodwise: Research Funding; Celgene: Speakers Bureau; MSD: Speakers Bureau. Socié: Alexion Pharmaceuticals, Inc.: Consultancy. Ciceri: GSK: Other: B-thalassemia gene therapy was developed by Fondazione Telethon and Ospedale San Raffaele and has been inlicenced by GSK that provides funding for the clinical trial, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.